Usefulness of EOB-MRI for hepatocellular carcinoma (HCC) pharmacotherapy
Nagasaki University Hospital
Drs. Ryu Sasaki and Kazuhiko Nakao, Dept. of Gastroenterology and Hepatology
DATE : 2021
Introduction

Patient’s background
Male; 60s; body weight: 57 kg; HCC
Assessment objectives
A nucleic acid analog was administered for chronic hepatitis B by the previous physician, and periodic monitoring was continued. Alpha-fetoprotein increase was found, and abnormalities were shown by abdominal ultrasonography, so the patient was referred to the authors’ hospital for thorough tests and additional treatment, and EOB-MRI was performed.
Contrast agent used
Gadoxetate disodium(Gd-EOB-DTPA) injection, 0.1 mL/kg
Case explanation
On the basis of the EOB-MRI results, the diagnosis made was HCC with associated tumor embolism as far as the portal vein main trunk. In the EOB-MRI hepatobiliary phase, the lesion did not show a heterogeneous high signal, and did show a homogeneous low signal, and it was considered possible that combination immunotherapy would be effective. Combination immunotherapy (combined with atezolizumab + bevacizumab) for nonresectable advanced liver cancer with associated Vp4 portal vein tumor embolism was therefore initiated. After completion of four cycles, although a remnant of the portal vein tumor embolism was found, the hepatic mass had markedly decreased in size, and radical resection (right lobectomy + portal vein thrombectomy) was performed after completion of the fifth cycle. At present, the patient has been monitored for the 14 months since surgery, without reinitiation of pharmacotherapy or recurrence.
Imaging findings
A multinodular lesion was found in the anterior segment of the right lobe of the liver, and part of it was branched.
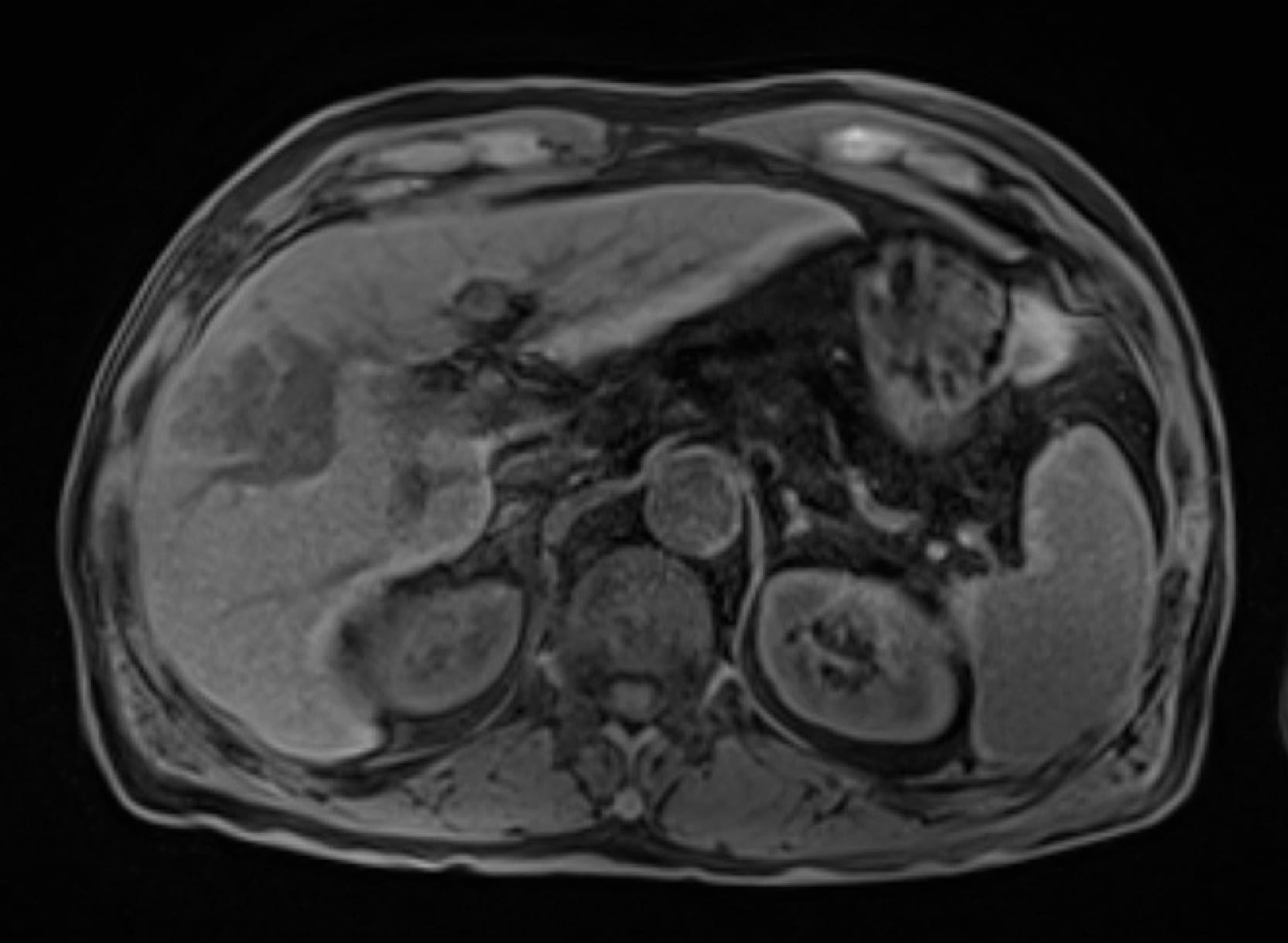
Fig. 1. Pretreatment simple EOB-MRI

A mass lesion in the anterior segment of the right lobe of the liver was slightly dark staining.
Fig. 2. Pretreatment early phase

The mass lesion in the anterior segment of the right lobe of the liver showed wash-out, with the branched part corresponding to the route of the portal vein, and the possibility of it being a portal vein tumor embolism was considered.
Fig. 3. Pretreatment late phase
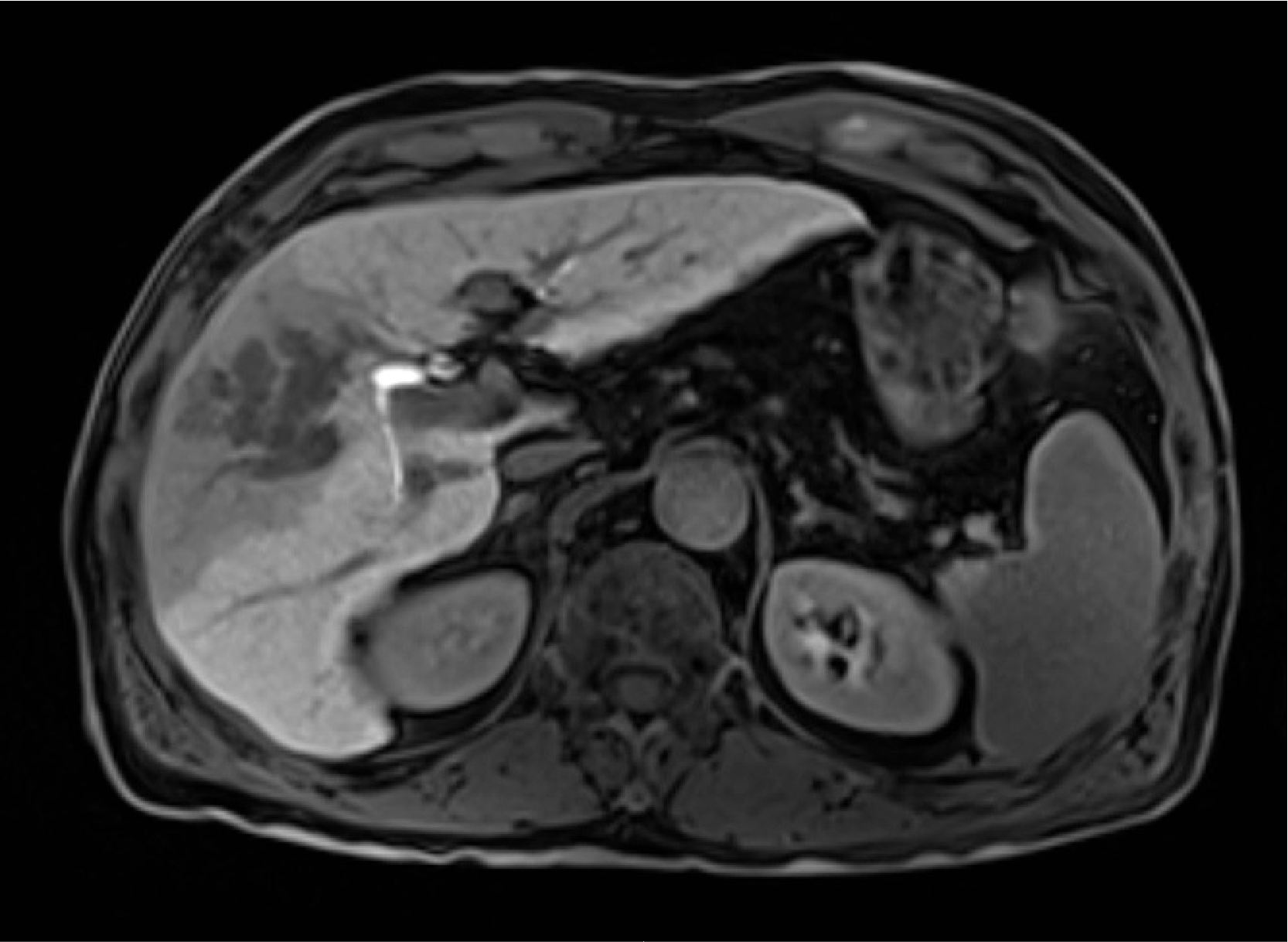
The mass lesion in the anterior segment of the right lobe of the liver showed a homogeneous low signal, and no heterogeneously high-signal region was found.
Fig. 4. Pretreatment hepatobiliary phase

Although part of the portal vein tumor embolism remained, the mass in the anterior segment of the right lobe of the liver showed marked reduction in size.
Fig. 5. Hepatobiliary phase after four treatment cycles
Photography protocol
| Imaging type | Photography sequence | Photography duration (s) | TE (msec) | TR (msec) | FA (deg) | Flipback (yes/no) | Fat sat (type) | ETL (number) | P-MRI (Reduction Factor) |
| Coronal section, T2-weighted imaging | HASTE | 17 | 80.00 | 728.0 | 120 | No | ー | ー | GRAPPA 3 |
| Dual echo | FLASH(3D-VIBE) | 18 | 1.38 2.46 | 4.2 | 10 | ー | ー | ー | CAIPIRINHA3 (p1s3) |
| Contrast agent administration | |||||||||
| Dynamic (artery) | FLASH(3D-VIBE) | 10 | 1.00 | 2.8 | 9 | ー | Fast Fat Ssturation | ー | CAIPIRINHA3 (p1s3) |
| Dynamic (venous) | FLASH(3D-VIBE) | 16 | 1.09 | 3.1 | 10 | ー | Fast Fat Ssturation | ー | CAIPIRINHA3 (p1s3) |
| T2WI | HASTE | 18 | 96.00 | 700.0 | 120 | No | ー | ー | GRAPPA 2 |
| Fat-suppressed, T2-weighted imaging | TSE | 15 x 2 | 76.00 | 3000.0 | 120 | No | SPAIR | 21 | GRAPPA 3 |
| DWI | EPI | Diaphragm synchronization | 52.00 | 2500.0 | ー | ー | SPAIR | ー | GRAPPA 2 |
| Hepatobiliary phase | FLASH(3D-VIBE) | 18 | 1.19 | 3.2 | 10 | ー | Fast Fat Ssturation | ー | CAIPIRINHA3 (p1s3) |
| Coronal section, hepatobiliary phase | FLASH(3D-VIBE) | 18 | 1.13 | 3.0 | 10 | ー | Fast Fat Ssturation | ー | GRAPPA 4 (p4) |
| Sagittal section, hepatobiliary phase | FLASH(3D-VIBE) | 17 | 1.13 | 3.0 | 10 | ー | Fast Fat Ssturation | ー | CAIPIRINHA3 (p1s3) |
| Imaging type | Holding breath (yes/no) | NEX (calculation number) | k-space | In-plane resolution (mm) | Slice thickness (mm) | FOV (mm) | Rectangu-lar FOV(%) | Phase direction (step number) |
| Coronal section, T2-weighted imaging | Yes | 1 | Linear | 0.94 x 0.94 | 6.0 | 360 | 75.0 | 288 |
| Dual echo | Yes | 1 | Linear | 1.13 x 1.13 | 3.0 | 360 | 75.0 | 168 |
| Contrast agent administration | ||||||||
| Dynamic (artery) | Yes | 1 | Centric | 1.25 x 1.25 | 3.0 | 360 | 75.0 | 162 |
| Dynamic (venous) | Yes | 1 | Centric | 1.13 x 1.13 | 3.0 | 360 | 75.0 | 180 |
| T2WI | Yes | 1 | Linear | 0.94 x 0.94 | 6.0 | 360 | 75.0 | 173 |
| Fat-suppressed, T2-weighted imaging | Yes | 1 | Linear | 1.13 x 1.13 | 6.0 | 360 | 75.0 | 195 |
| DWI | No | 4 | Linear | 2.43 x 2.43 | 6.0 | 360 | 75.0 | 78 |
| Hepatobiliary phase | Yes | 1 | Centric | 1.13 x 1.13 | 2.0 | 360 | 75.0 | 168 |
| Coronal section, hepatobiliary phase | Yes | 1 | Linear | 1.13 x 1.13 | 3.0 | 360 | 75.0 | 240 |
| Sagittal section, hepatobiliary phase | Yes | 1 | Centric | 1.13 x 1.13 | 3.0 | 360 | 75.0 | 168 |
| Imaging type | Read direction (matrix number) | Actual scan (%) | Slice Gap (mm) | Slice number | Three-dimensional partition number | Three-dimensional actual scan (%) | 3D over sampling(%) |
| Coronal section, T2-weighted imaging | 384 | 75 | 1.5 | 23 | ー | ー | ー |
| Dual echo | 320 | 70 | ー | ー | 80 | 60 | 20.0 |
| Contrast agent administration | |||||||
| Dynamic (artery) | 288 | 75 | ー | ー | 80 | 50 | 20.0 |
| Dynamic (venous) | 320 | 75 | ー | ー | 80 | 60 | 20.0 |
| T2WI | 384 | 60 | 1.8 | 26 | ー | ー | ー |
| Fat-suppressed, T2-weighted imaging | 320 | 81 | 1.8 | 26 | ー | ー | ー |
| DWI | 148 | 70 | 1.8 | 26 | ー | ー | ー |
| Hepatobiliary phase | 320 | 70 | ー | ー | 120 | 50 | 33.3 |
| Coronal section, hepatobiliary phase | 320 | 75 | ー | ー | 72 | 65 | 11.1 |
| Sagittal section, hepatobiliary phase | 320 | 70 | ー | ー | 104 | 64 | 23.1 |
Devices used and contrast conditions
| MRI device | SIEMENS MAGNETOM Vida |
| Automatic injection device | Sonic Shot 7 (Nemoto Kyorindo) |
| Workstation | FUJIFILM SYNAPSE VINCENT |
| Contrast conditions | Dose (mL) | Administration rate (mL/s) | Photography timing | |
| Gadoxetate disodium(Gd-EOB-DTPA) | 5.7 | 1.5 | The details of bolus-tracking are shown in the Comments column. | |
| Physiological saline solution for flushing | 20 | 1.5 |
Dynamic EOB-MRI started the photography of a coronal-section CARE Bolus sequence, after which contrast agent injection was initiated. After real-time monitoring, and approximately 7 s after the contrast agent had reached the pulmonary artery, imaging was performed during the arterial phase (two consecutive 10-s periods during one breath-holding episode), followed by imaging at three time-points during the venous phase (immediately, 60 s after, and 120 s after completion of the arterial phase). Imaging in the hepatobiliary phase was performed from 20 minutes after injection of the contrast medium.
Usefulness of Gadoxetate disodium(Gd-EOB-DTPA) contrast MRI with this patient
It was shown by EOB-MRI that the lesion was HCC with associated portal vein tumor embolism, not showing a heterogeneous high signal, and combined immunotherapy (combined with atezolizumab + bevacizumab) was initiated. The EOB-MRI hepatobiliary phase is known to show imaging biomarkers for Wnt/β-catenin mutations in HCC (Ueno et al., J Hepatol 61: 1080-1087, 2014), and it has been pointed out that heterogeneously high-signal lesions may show poor responses to combined immunotherapy (Sasaki et al., Cancers 14: 827, 2022). Although this does not ensure therapeutic effect, with this patient a homogeneously low signal was shown in the hepatobiliary phase, and the combination immunotherapy is expected to show therapeutic efficacy.
The “Indications and effects” for Gadoxetate disodium(Gd-EOB-DTPA) Injection Syringe are shown below, and there is no indication predicting the therapeutic efficacy of the drug.
Excerpt from package insert
4. Indications and effects
Hepatic tumor imaging with magnetic resonance computed tomography
- *The case introduced is just one clinical case, so the results are not the same as for all cases.
- *Please refer to the Package Insert for the effects and indications, dosage and administration method, and warnings, contraindications, and other precautions with use.


